How a glomerulus in vitro model can accelerate drug development
Glomerular damage due to drug toxicity or chronic kidney disease is difficult to study because there are no suitable in vitro models that resemble the human tissue. Typically, the limiting factor is obtaining and culturing high quality functional podocytes that could support high throughput and high content screening for drug development.
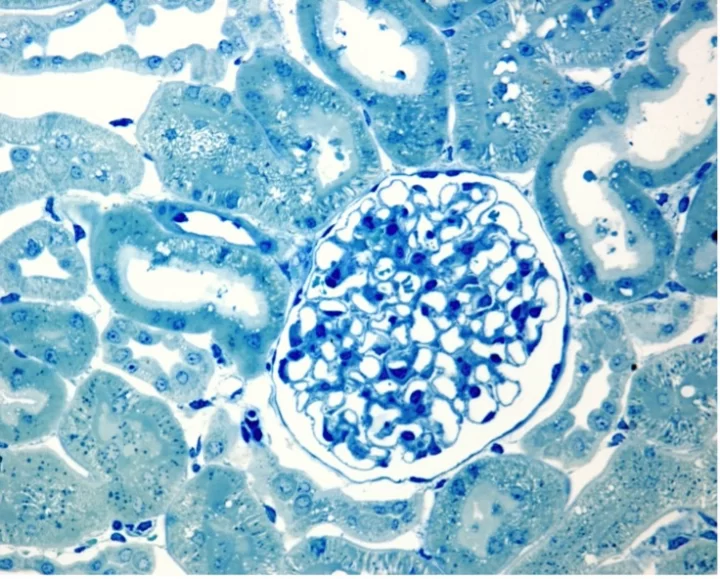
The glomerulus is the part of the kidney involved in the filtration of solutes and waste from the blood. Damage to the glomerulus by diabetes mellitus, hypertension, glomerulonephritis, or cystic kidney disease eventually leads to kidney failure. In these circumstances, there are very limited therapeutic options, and the pathological mechanisms are not yet well established. Glomerular damage is difficult to understand and difficult to study.
Why is the glomerulus so difficult to study?
The glomerulus is extremely difficult to study due to the lack of suitable in vitro models that can recapitulate the complexity of the tissue. Therefore, an in vitro model of the glomerulus that is high throughput is desperately needed to accelerate drug development and early assessment of drug safety and nephrotoxicity.
Do glomerular in vitro models exist?
Currently some in vitro models of the glomerulus exist, but they have limitations.
Immortalized cells are cost-effective and well-established, but they are physiologically inaccurate and have poor predictivity of in vivo outcomes. Human induced pluripotent stem cells (iPSCs) have a robust ability of self-renewal, however, they display immature and not fully differentiated phenotypes. Three-dimensional (3D) scaffolds that use extracellular matrix (ECM) derived biomaterials allow the formation of structures with biological relevance that can replicate the glomerular basal membrane (GBM) and the ECM microenvironment. Unfortunately, these 3D scaffolds can have limited physiological resemblance and are poorly developed when it comes to the glomerulus. All these models, whether 2D or 3D, lack the dynamic stimuli that the tissue is exposed to.
In the past decades, organ-on-chip platforms, biometric membranes, organoids, and a combination of these are being developed as they hold the promise of recapitulating the complexity of the glomerulus in vitro. Organ-on-chip platforms aim at having improved physiological accuracy through compartmentalization and fluid flows. However, they are limited in cell-cell and cell-ECM interactions. So far, there are only a small variety of biomaterials that can permit their fabrication, also limiting the type of assays that they could be subjected to and therefore the outputs that can be obtained from these platforms. Finally, organoids represent scaffold-free 3D structures that recapitulate the tissue architecture. Though cells are in proximity, these cells present immature phenotypes and cell-ECM interactions are restricted.
None of the existing models are high throughput.
In the past decades, organ-on-chip platforms, biometric membranes, organoids, and a combination of these are being developed as they hold the promise of recapitulating the complexity of the glomerulus in vitro.
What would be needed for a high throughput high content screening model of the glomerulus?
In short, scalability and standardization.
Modern technologies could potentially allow the automated fabrication of glomerular models using 3D printing and laser ablation to have a high throughput (HT) glomerular model that can be used for high content screening. Scalability will require standardization not only of the fabricated constructs but also of protocols for obtaining and seeding the human cells onto those constructs, maturing those cells in vitro and validating the model.
Are there any bottlenecks in the generation of glomerulus models?
Podocytes are often the limiting factor in glomerular models since they lack proliferative capacity and hold high specificity. Filtration quality and specificity depends on the podocytes and glomerular endothelial cells that form the glomerulus filtration barrier (GFB). Disruptions or alterations in podocytes primary and secondary foot processes, or in glomerular endothelial cells could have major consequences for the filtration process, highlighting how crucial it is to model and characterize cells in vitro when developing a glomerulus model.
A reliable method for obtaining physiologically relevant podocytes is necessary to accelerate drug development.
How can Newcells Biotech help?
Newcells is a pioneer in building and developing complex in vitro models for drug development and testing. We are developing an in vitro podocyte model that will be available in September 2022. A mutli-cellular glomerulus model containing podocytes, endothelial cells and mesangial cells is also in development. Newcells also has the capability to build new models and generate micro physiological systems (MPS) from a range of tissues.
Share on social media:
Don't miss out on our latest innovations: follow us on Linkedin
Newcells Biotech
11th August, 2022
Products
Kidney